Home Articles AIIMS releases guidelines for early detection, prevention of mucormycosis, Covid ward on...
KEY STORY
-
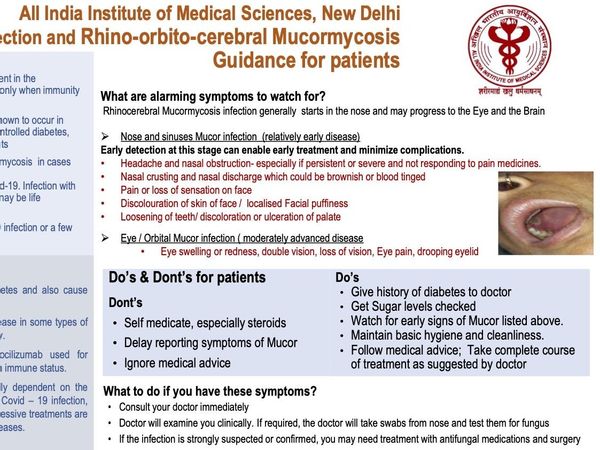
AIIMS’ latest guidelines call for the identification of high-risk patients in the Covid ward to detect and treat patients of deadly mucormycosis on time.
-
The guidelines also list out signs for which patients and their caretakers must keep a lookout for early detection of mucormycosis so that medical staff is alerted on time and timely treatments save lives.
-
AIIMS’s Dr Rajendra Prasad Centre for Ophthalmic Studies Wednesday night released guidelines for early detection and prevention of mucormycosis in AIIMS’s Covid Ward.
Who are the “high-risk” patients in the Covid ward?
The AIIMS pamphlet online says many patients with Mucor are noted to be RTpcr +ve at >10 days from onset. This may represent immunocompromise related persistence of COVID infection.
According to doctors, cases of mucormycosis, also known as black fungus, are being seen among Covid patients who were administered steroids to treat symptoms, and particularly among those who are suffering from diabetes and cancer. Medical experts have pointed to strong links between diabetes and infection.
Also, Covid-19 has a tendency to worsen diabetes and also precipitate diabetes in previously normal individuals.
The “high risk” Covid patients physicians have been asked to identify are:
-
Patients with uncontrolled diabetes, diabetic ketoacidosis, and diabetics on steroids or tocilizumab
-
Patients on immunosuppressants or anticancer treatment, and patients with a chronic debilitating illness
-
Patients on high dose steroids and/or long duration of steroids or tocilizumab
-
Severe Covid cases
-
Patients on oxygen support—nasal prongs, by mask, or on a ventilator
Ophthalmologists have been asked to conduct a baseline examination of these high-risk patients, followed by weekly examinations till the time of discharge.
The guidelines also stress on follow-up examination, depending on the patient’s condition either every two weeks for six weeks, or once every month for three months.
What do patients and their caretakers need to look out for?
Mucormycosis has a typical set of symptoms:
-
Abnormal black discharge or crusty dryness, or bleeding from the nose
-
Nasal blockage
-
Headache or eye pain
-
Swelling around the eyes, double vision, redness of the eye, loss of vision, difficulty in the closing eye, inability to open the eye, prominence of the eye
-
Facial numbness or tingling sensation, difficulty in chewing or opening the mouth
The AIIMS COVID Portal too has a complete brochure on Mucormycosis, recognition of onset and treatment by doctors.
Therein are listed sentinel signs/symptoms to be monitored in patients admitted to the COVID-19 wards.
Nose and sinuses showing mucor infection are the relatively early stages of the infection, it says; adding that timely detection at this stage can enable early treatment and minimize complications.
At the moderately advanced stage comes the Eye/Orbital mucor infection.
Intracranial infection is considered a very advanced disease when cavernous sinuses are involved and cranial nerve palsies occur.
Patients’ relatives or caretakers are advised to help the patient consciously conduct regular self-examinations. These include a full face examination in daylight for facial swelling—especially of the nose, cheeks, around the eyes—or black discolouration, hardening, and pain on touch; as well as oral and nasal examinations using a torch to check for blackening and swelling inside the mouth or nose.
If a patient identifies any of these signs, what must they do?
They must immediately consult an ENT doctor or ophthalmologist for their treatment, and not self-medicate with steroids, antibiotics or antifungal drugs. Apprise the doctor about your medical conditions. Mention your blood sugar levels history, immunosuppressive treatments if any, etc.
Strict control and monitoring of blood sugar should be maintained.
No self-medication with steroids, antibiotics, anti-fungal.
Get an MRI CT scan with contrast – paranasal sinuses and orbit, if the doctor advises.
Please note: Stay vigilant even weeks after recovering from COVID-19 as Mucor infection may occur during COVID-19 infection, or after a few weeks of apparent recovery from it.
Disclaimer: Tips and suggestions mentioned in the article are for general information purpose only and should not be construed as professional medical advice. Always consult your doctor or a dietician before starting any fitness programme or making any changes to your diet.